Diabetes affects your body from head to toe. That includes your eyes. The most common and most serious eye complication of diabetes is diabetic retinopathy, which may result in poor vision or even blindness.
Retinopathy is the medical term for damage to the many tiny blood vessels (capillaries) that nourish the retina, the area at the back of your eye that captures light and relays information to your brain. These blood vessels are often affected by the high blood sugar levels associated with diabetes.
The longer you have diabetes, the more likely it is you’ll develop diabetic retinopathy. After having type 1 diabetes (formerly called juvenile or insulin-dependent diabetes) for 20 years, almost everyone with this condition has some degree of retinopathy. After the same number of years, more than 60 percent of people with type 2 diabetes (formerly called adult-onset or noninsulin-dependent diabetes) have some degree of retinopathy. Initially, most people with diabetic retinopathy experience only mild vision problems. But the condition can worsen and threaten your vision.
The threat of blindness is scary. But there’s more cause for hope than for alarm. With early detection and treatment, the risk of severe vision loss from diabetic retinopathy is less than 5 percent. And you can take steps to protect your sight if you have diabetes.
Start with a yearly eye examination. Work to keep your blood sugar and blood pressure under the best possible control.
Signs and Symptoms
In the early, most treatable stages of diabetic retinopathy, you usually experience no visual symptoms or pain. The disease can even progress to an advanced stage without any noticeable change in your vision.
Symptoms of diabetic retinopathy can include:
- “Spiders,” “cobwebs” or tiny specks floating in your vision.
- Dark streaks or a red film that blocks vision.
- Vision loss, usually in both eyes, but more so in one eye.
- Blurred vision that may fluctuate.
- A dark or empty spot in the center of your vision.
- Difficulty adjusting from bright light to dim light.
Causes
If you have diabetes, your body doesn’t use sugar (glucose) properly. Sugar in the blood is vital to your health because it’s a main source of energy for your body’s cells. But too much sugar in the blood can cause a host of problems. For one thing it damages the capillaries that supply nutrients to organs and tissues such as the brain, the nerves, the kidneys and the eyes. Damage to the capillaries in your eyes occurs in diabetic retinopathy.
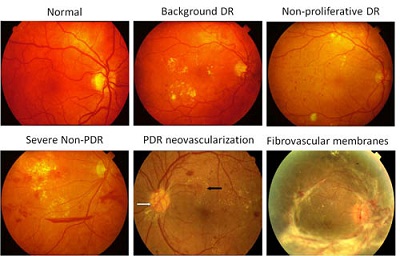
Diabetic retinopathy occurs in two types. Usually both eyes are affected, although the disease may be more advanced in one eye.
Nonproliferative diabetic retinopathy (NPDR)
This type, also called background diabetic retinopathy, is an early stage of the disease. It’s the most common type of retinopathy, and symptoms are often mild.
In NPDR the walls of blood vessels in the retina weaken. Tiny bulges called microaneurysms (mi-kro-AN-u-riz-umz) protrude from the vessel walls. Another term for this is outpouching. The microaneurysms may begin to leak, oozing fluid and blood into the retina. As NPDR progresses, other signs of damage appear. These include patches of swollen nerve fibers, which are called cotton wool spots because they look like fluffy wisps of cotton.
Mild NPDR may not affect your ability to see clearly. Vision problems from more severe NPDR are usually the result of swelling (edema) of the central part of the retina (macula) or the closing of capillaries, which reduces blood flow to the macula (macular ischemia). When the macula can’t function properly, your central vision decreases. Your peripheral vision usually remains normal.
Proliferative diabetic retinopathy (PDR)
This is the more advanced form of the disease. About half the people with very severe NPDR progress to PDR within 1 year. Retinopathy becomes proliferative when abnormal new blood vessels grow (proliferate) on the retina or the optic nerve. The blood vessels also grow into the vitreous, the clear, jelly like substance that fills the center of the eye.
This abnormal growth follows the widespread closing of capillaries in the retina due to high blood sugar levels. The condition can cause vision loss affecting both your central and peripheral vision. The new blood vessels may leak blood into the vitreous, which clouds or even blocks your vision. Other complications include detachment of the retina due to scar tissue formation and a form of Glaucoma associated with the growth of abnormal blood vessels on the iris, the pigmented portion of the eye surrounding the pupil.
Blurred vision in diabetes
Blurred vision is commonly brought on by fluctuations in blood sugar. Prolonged periods of elevated blood sugar cause sugar and its breakdown products to accumulate in the lens. This accumulation sucks up water and makes the lens swell, resulting in nearsightedness — meaning distant objects appear blurry to you. The nearsightedness subsides once your blood sugar is brought under steady control.
Blurred vision can also be caused by macular edema or swelling, regardless of your blood sugar level. This is a cause for greater concern because macular edema often develops in people with diabetic retinopathy. The swelling may fluctuate during the day, making your vision get better or worse. If blood vessels in your eye are hemorrhaging, you might notice spots floating in your field of vision temporarily. These small spots are often followed within a few days or weeks by larger spots or clouds, which are caused by more massive hemorrhaging.
Risk Factors
Having diabetes puts you at risk of retinopathy, whether you have type 1 or type 2 diabetes. Your risk increases the longer you have the disease. People with type 1 diabetes are at especially high risk because they usually become diabetic at a young age. If you were over 30 when you first got diabetes, your risk is lower, but for some people in this group, retinopathy may be the first sign of diabetes.
Whatever your age, if you need to take insulin, your risk of retinopathy is higher.
Other risk factors for diabetic retinopathy include:
- Poorly controlled blood sugar levels.
- Kidney disease.
- High blood pressure.
- High blood fats — elevated levels of low-density lipoprotein cholesterol and triglycerides.
- Pregnancy. Women with type 1 diabetes who become pregnant have about a 10 percent risk of developing NPDR. Women who already have NPDR when they become pregnant tend to experience a progression of the disease, although it may improve after delivery. Less than 10 percent of pregnant women with mild NPDR develop PDR.
- Obesity.
When to Seek Medical Advice
A common misconception among people with diabetes is, “If I can see well, there’s nothing wrong with my eyes.” This is false confidence. The majority of people who lose their sight because of diabetic retinopathy do so because they didn’t seek early medical attention. It bears repeating: If you have diabetes, you are at risk even if you don’t have any apparent vision problems. For this reason regular eye examinations are essential.
When and how often do you need your eyes checked? The American Academy of Ophthalmology recommends the following schedule:
- If you received a diagnosis of diabetes before age 30, have a comprehensive eye exam by the time diabetes has been present for 5 years or at age 10, whichever is later.
- If you received a diagnosis at age 30 or older, have a baseline eye exam at the time of the diagnosis.
- If you’re a woman with diabetes who’s pregnant or intending to become pregnant, have an eye exam before conception or early in the first trimester and thereafter every 3 months.
- After the initial exam, have your eyes checked every year, unless you have eye conditions that require more frequent monitoring.
- See your eye doctor promptly if your eyes become painful and red, your vision decreases, or you see floaters or light flashes. If diabetic retinopathy is found, the course of treatment depends on the severity of the condition and whether your vision is currently impaired or threatened by the retinal changes.
Screening and Diagnosis
Your eye doctor will likely diagnose diabetic retinopathy, either nonproliferative or proliferative, if an eye examination reveals any of the following:
- Leaking blood vessels.
- Microaneurysms.
- Swollen retina.
- Fatty deposits (exudates) on the retina.
- Areas of nerve fiber damage (cotton wool spots).
- Changes in blood vessels, such as closures, beading, loops.
- Formation of new blood vessels (neovascularization).
- Retinal hemorrhage.
- Vitreous hemorrhage.
- Scar tissue formation with retinal detachment.
As part of an eye examination, your doctor may use a procedure called fluorescein angiography to assess damage to normal blood vessels and note the formation of abnormal blood vessels.
In fluorescein angiography, your doctor injects a dye into a vein in your arm. As the dye circulates through your eyes, the blood vessels in your retina stand out as bright yellow. A camera takes flash pictures every few seconds for several minutes, providing your doctor with useful images.
Complications
The abnormal growth of new blood vessels in proliferative diabetic retinopathy doesn’t resupply the retina with a normal blood flow. Instead, these vessels may produce other complications:
Vitreous hemorrhage. The new blood vessels may bleed (hemorrhage) into the vitreous. If the amount of bleeding is small, you might see only a few dark spots or floaters. In more severe cases, blood can completely fill the vitreous cavity and block all of your vision. Vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood eventually clears from the eye — usually within a few months — and your vision returns to its previous clarity, unless your retina is damaged.
- Traction retinal detachment. The new blood vessels are often accompanied by the growth of scar tissue. The scar tissue eventually shrinks. As it shrinks it pulls the retina away from the back wall of the eye. This causes blank or blurred areas in your field of vision.
- Neovascular glaucoma. The proliferation of blood vessels on the retina may be accompanied by the growth of abnormal new blood vessels on the iris. This can interfere with the normal flow of fluid out of the eye and cause pressure in the eye to build up. The result is neovascular glaucoma, a serious complication of diabetic retinopathy that can cause pain, vision loss and, if not treated successfully, the loss of the eye.
Treatment
If you have mild NPDR, you may not require treatment right away. However, your eye doctor will want to closely monitor your retina. More advanced forms of retinopathy often require prompt surgical treatment.
The two main treatments for diabetic retinopathy are photocoagulation and vitrectomy. In a majority of cases, these treatments are effective and slow or stop the progression of the disease for some time. But they’re not a cure. Because diabetes continues to affect your body, you may experience further retinal damage and vision loss at a later time.
Photocoagulation
The goal of photocoagulation is to stop the leakage of blood and fluid in the retina and thus slow the progression of diabetic retinopathy. The decision to use the procedure depends on the type of diabetic retinopathy you have, its severity and how well it may respond to treatment.
- Your doctor may recommend photocoagulation if you have:
- Macular edema, a swelling that involves or threatens the center of the retina.
- Severe NPDR, especially if you have type 2 diabetes.
- PDR.
- Neovascular glaucoma.
In photocoagulation a high-energy laser beam creates small burns in areas of the retina with abnormal blood vessels to seal any leaks. The procedure takes place in your doctor’s office or in an outpatient surgical center. Before surgery, your eye doctor dilates your pupil and applies anesthetic drops to numb your eye. In some cases he or she numbs your eye more completely by injecting anesthetic around and behind your eye.
First, your chin and forehead are rested in an examination device called a slit lamp. This is a microscope that uses an intense line of light (slit) to allow your doctor to clearly view portions of your eye. Then, your doctor places a medical contact lens on your cornea — the layer of clear tissue at the front of your eye — to help focus laser light onto the sections of the retina to be treated. Fluorescein angiographic photographs may serve as maps to show where the laser burns should be placed. During the procedure you may see bright flashes from the short bursts of high-energy light.
To treat macular edema, the laser is focused on spots where blood vessels are leaking near the macula. The doctor makes “spot welds” to stop the leakage. If the leaks are small, the laser is applied directly to specific points where the leaks occur (focal laser treatment). If the leakage is widespread, laser burns are applied in a grid pattern over a broad area (grid laser treatment).
Shortly after laser treatment, you can usually return home, but you won’t be able to drive, so make sure to arrange for a ride. Your vision will be blurry for about a day. You may have some eye pain or a headache and be sensitive to light. An eye patch and over-the-counter pain relievers should help to ease the discomfort. Even when laser surgery is successful in sealing the leaks, new areas of leakage may appear later. For this reason you’ll have follow-up visits and, if necessary, additional laser treatments.
Immediately following laser surgery to treat macular edema, small spots caused by the laser burns may appear in your visual field. The spots generally fade and disappear with time. If you had blurred vision from macular edema before surgery, you may not regain complete normal vision.
Vitrectomy
Often a vitreous hemorrhage clears up on its own. But photocoagulation treatment is impossible if the hemorrhage is massive and doesn’t clear. That’s when a vitrectomy becomes necessary to restore sight or prevent total loss of vision. Early vitrectomy is especially beneficial for people with complications of type 1 diabetes.
In this procedure your surgeon uses delicate instruments to remove the blood-filled vitreous. A vitreous cutter cuts the tissue and removes it, piece by piece, from your eye. A tube (infusion cannula) replaces the volume of removed tissue with a balanced salt solution to maintain the normal shape and pressure of the eye. A light probe illuminates the inside of the eye. The surgeon performs the procedure while looking through a microscope suspended over the eye. In this way the vitreous blood is removed to re-establish clear vision.
A vitrectomy is also used to remove scar tissue when it begins to pull the retina away from the wall of the eye. This allows a detached retina to settle back and flatten out. Your eye doctor may decide not to operate on a retina detached by scar tissue if the detachment is located away from the macula and doesn’t appear to be progressing.
During a vitrectomy the surgeon may also use a laser probe to perform a procedure called panretinal photocoagulation. This can prevent renewed growth of abnormal blood vessels and bleeding.
Vitrectomy is usually done under local anesthesia on an outpatient basis. Your eye will be red, swollen and sensitive to light for some time after surgery. For a short time afterward, you’ll need to wear an eye patch and apply medicated eye drops to help the healing.
Full recovery may take weeks. When a vitrectomy is done for PDR with a massive vitreous hemorrhage, some blood may remain in your eye, or fresh bleeding may occur. It may take several weeks for your sight to clear.
Following a vitrectomy for traction retinal detachment or vitreous hemorrhage, vision improves in most people. When surgery fails to improve vision, it’s usually because of irreparable damage to the retina from diabetes. But at times it can be due to complications of the surgery, recurring vitreous bleeding, retinal detachment or the formation of new blood vessels on the iris (neovascular glaucoma).
Panretinal photocoagulation
For proliferative diabetic retinopathy, doctors use a form of laser surgery called panretinal or scatter photocoagulation. With this technique the entire retina except the macula is treated with randomly placed laser burns. The treatment causes the abnormal
new blood vessels to shrink and disappear. Thus it reduces the chances of vitreous hemorrhage. Panretinal photocoagulation is usually done in two or more sessions. The treatment significantly reduces the risk of severe vision loss.
If the treatment is extensive, you may notice some loss of peripheral vision afterward. Panretinal photocoagulation is a trade-off. Some of your side vision is sacrificed to save as much of your central vision as possible. You may also notice more difficulties with your night vision and temporary blurring of your central vision. Panretinal photocoagulation doesn’t always stop loss of vision from diabetic retinopathy, even with repeated treatments.
Read More
Read More
Read More
Read More







