| Glaucoma isn’t one disease. Instead, it’s a group of diseases that cause damage to the optic nerve. In most cases, this damage is the result of increased pressure within your eye. As the optic nerve deteriorates, the patient gradually loses the ability to see to the side (peripheral vision). With time your central vision may begin to decrease as well. If Glaucoma isn’t treated, it eventually may lead to total blindness. In fact, Glaucoma is the second most common cause of blindness. That’s because Glaucoma often gives no warning sign until permanent damage has already occurred. In most cases the onset is so gradual you’re not aware you’ve lost some of your peripheral vision.There are several types of Glaucoma, including primary open-angle glaucoma, angle-closure glaucoma, congenital glaucoma and secondary glaucoma. Primary open-angle glaucoma develops slowly and painlessly when normal eye fluid known as aqueous humor doesn’t drain properly, causing pressure to build up within your eye. It accounts for 60 percent to 70 percent of all Glaucoma cases.About 10 percent of people with Glaucoma have angle-closure glaucoma, which occurs suddenly and often causes dramatic symptoms. This type of Glaucoma is a medical emergency and requires immediate treatment. A much smaller number of people have congenital glaucoma, which is present at birth, or secondary glaucoma, which results from trauma, chronic steroid use or disease. Still, the news about Glaucoma is encouraging. When it’s detected and treated early, Glaucoma need not cause blindness or even severe vision loss for most people.Signs and Symptoms The signs and symptoms of Glaucoma vary, depending on the type of Glaucoma.Primary open-angle glaucoma Primary open-angle glaucoma often goes undetected for years. Pressure within the eye increases gradually, with no early warning signs. But eventually, you lose more and more of your side vision until only a narrow section of your visual field remains clear. This type of Glaucoma tends to affect both eyes, although you may have symptoms in just one eye first. In addition to reduced peripheral vision, the signs and symptoms of primary open angle glaucoma may include:
Angle-closure glaucoma
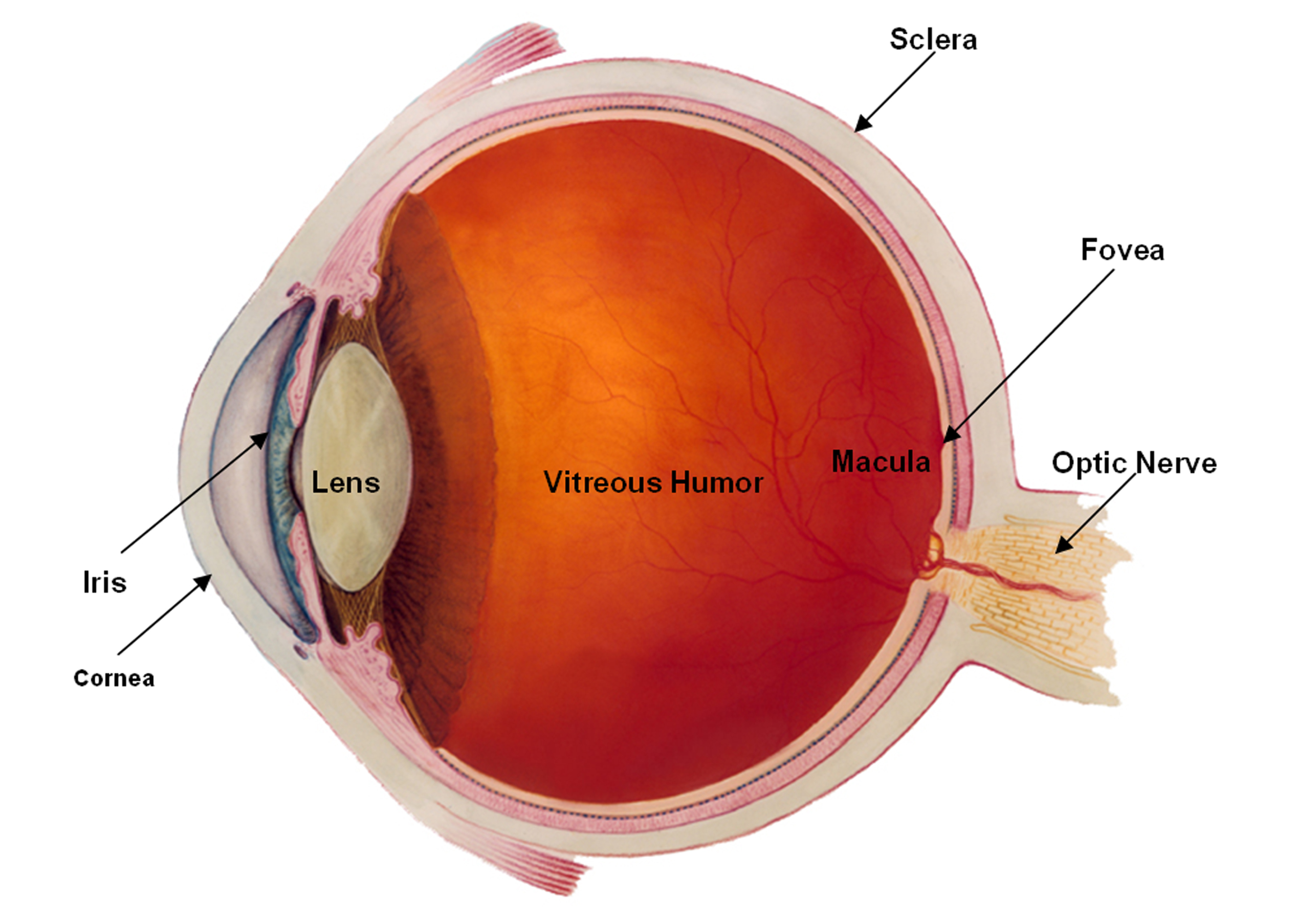
Secondary glaucoma Causes The internal structures of your eye are nourished by a clear fluid called the aqueous humor. This fluid circulates from behind your iris through the dark opening in the center of your eye (pupil) and into the space between your iris and your cornea. The aqueous humor not only nourishes your eyes but also exerts a constant pressure (intraocular pressure, or IOP) that helps maintain your eyes’ shape. Healthy eyes constantly produce aqueous humor. To keep from building up in the eye, the fluid drains primarily through what is called the trabecular meshwork. This drainage occurs in a “drainage angle” located at the point where your iris and cornea meet. From here, the excess fluid flows into a channel (Schlemm’s canal), and then into a system of small veins on the outside of your eye. Primary open-angle glaucoma
In some people the narrow drainage angle may simply be a structural problem. In others it may be the result of aging. Generally, as you age the lens in each eye gradually becomes larger, pushing your iris forward and narrowing the angle between your iris and cornea.
Secondary glaucoma
Risk Factors
When To Seek Medical Advice Primary open-angle glaucoma gives few warning signs until permanent damage has already occurred. That’s why regular eye exams are the key to detecting glaucoma early enough for successful treatment. It’s best to have routine eye checkups every 2 to 4 years after age 40 and every 1 to 2 years after age 65. Don’t wait for symptoms of any kind to occur. If you have one or more risk factors of glaucoma, talk to your doctor about scheduling regular eye exams. Your doctor can perform some tests, but others need to be done by an eye care specialist. In addition, be alert for signs of an acute angle-closure glaucoma attack, such as a severe headache or pain in your eye or eyebrow, nausea, blurred vision or rainbow halos around lights. If you experience any of these symptoms, seek immediate care at your local hospital emergency room. Screening And Diagnosis A simple, painless testing procedure known as tonometry can alert you and your physician to the possibility you may have Glaucoma. Tonometry measures the pressure within your eyeball. Normal intraocular pressure ranges from 10 to 21 millimeters of mercury. If your pressure is higher, your ophthalmologist can perform further tests to help determine whether you have Glaucoma. Air-puff tonometry Air-puff tonometry uses air to measure eye pressure. It does this by measuring the amount of force needed to indent your eye. This test is useful for preliminary Glaucoma screenings. Applanation tonometry An applanation tonometer is a sophisticated device that’s usually fitted to a slit lamp, a common instrument for eye examination. For this test, your eyes will be anesthetized with drops and the tonometer placed directly on your eye. The pressure readings from this test are extremely accurate. Your ophthalmologist may use an instrument called an ophthalmoscope to examine the back of your eye (fundus) and check the health of the fibers in your optic nerve. Damaged fibers may be asymmetrical or pale in color. Your doctor may also use a combination of laser light and computers to create a three-dimensional image of your optic nerve. This can reveal very slight changes that may indicate the beginnings of Glaucoma. Visual field tests Glaucoma gradually diminishes your ability to see to the side. That’s why your ophthalmologist may recommend perimetry tests to check your peripheral vision. Some of these tests, which involve watching a monitor with hundreds of flickering lights, can be quite complex. Yet perimetry tests are still the best method for measuring peripheral vision. If you have optic nerve damage, you may need visual field testing as often as every 1 to 4 months for a time. Other tests To distinguish between primary open-angle and angle-closure glaucoma, your ophthalmologist may use an instrument known as a gonioscope to inspect the drainage angle between your cornea and iris. You may not need any treatment if your eye pressure is only slightly elevated and there’s no damage to your optic nerve. Instead, your doctor may choose to monitor your condition with regular eye exams. But if you have signs of optic nerve damage, treatment can help slow its progression. Unfortunately, it’s not currently possible to reverse damage that has already occurred. Most people have good results with Glaucoma medication, but some may need surgery instead. Medications for Glaucoma Most Glaucoma medications are applied directly to your eyes in the form of drops, although a few may be taken orally. Because a portion of the drops may be absorbed into your bloodstream, you sometimes may have side effects unrelated to your eyes. In addition, some medications may lose their effectiveness over time. In that case, you may need to change or add medications or have surgery to control your Glaucoma. Furthermore, because Glaucoma rarely causes symptoms in its early stages, you may not notice any change in your vision when you start using medication. Still, it’s extremely important to follow your treatment plan exactly as your doctor prescribes. Skipping even a few doses of medication can cause your Glaucoma to become worse. If you have trouble with your treatment plan, tell your doctor. Surgery for Glaucoma When medications aren’t effective or well tolerated, surgery may be an option. Keep in mind that surgery doesn’t cure Glaucoma. As a result, you may need to keep using antiglaucoma medications even after surgery. In some cases, you may need a second operation.
Medications and surgery for acute glaucoma Doctors may administer several different medications during an attack of acute glaucoma in an effort to reduce eye pressure as quickly as possible. Once your eye pressure is brought under control, you may have an emergency operation known as an iridotomy to create a drainage hole in your iris. This surgery is now almost exclusively performed with lasers, which allow specialists to form an opening without making an incision in your eye. Laser iridotomy is an outpatient procedure that avoids many of the risks of traditional surgery. After treatment you can usually resume your normal activities right away. Treatment for low-tension glaucoma Although eye pressure in this type of Glaucoma is normal, treatment with standard antiglaucoma medications seems to slow the progress of the disease. Prevention There is no known way to prevent Glaucoma, but regular checkups can help detect the disease in its early stages before irreversible damage has occurred. As a general rule, have eye exams every 2 to 4 years if you’re between the ages of 40 and 65. It’s best to have your eyes examined every 1 to 2 years if:
You may need even more frequent check-ups if you’ve been diagnosed with abnormally high intraocular pressure or have a history of serious eye injury. |
Read More
Read More
Read More
Read More






